Tibialis Posterior Dysfunction
The most common cause of a flatfoot deformity in an otherwise healthy person is dysfunction of the tibialis posterior tendon. The tibialis posterior tendon is the main stabilising muscle of the arch of your foot.
The diagnosis of tibialis posterior tendon dysfunction at Erica dash podiatry is largely a clinical one.
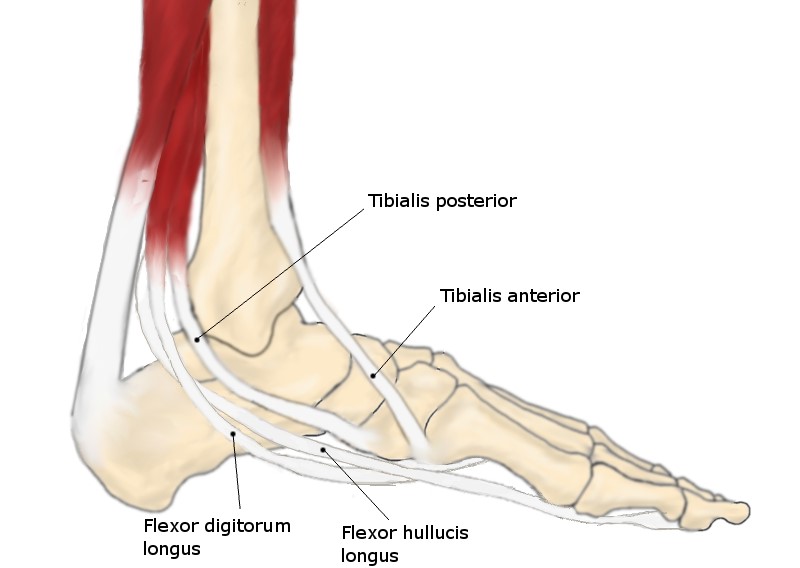
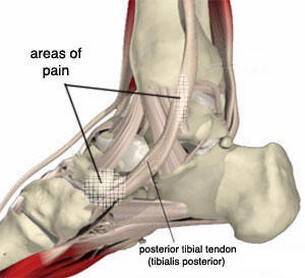
Typically, there will be pain and swelling behind the medial malleolus (The bump on the inside of the ankle) and along the instep.
As this condition progresses there can be a flattening of the arch and a valgus heel position can develop. The ability to walk is hampered and balance is usually adversely affected.
Standing on 1 leg can be difficult.
Tibialis posterior dysfunction is often poorly diagnosed by some health practitioners and by the time patients present to a specialist foot and ankle clinic they have had the condition for several years and have unsuccessfully consulted numerous doctors.
An increased awareness of the existence of tibialis posterior should serve to help patients with earlier referral and treatment and by limiting the amount of disability they experience.
Rather than tendon inflammation, the process is one of tendon degeneration.
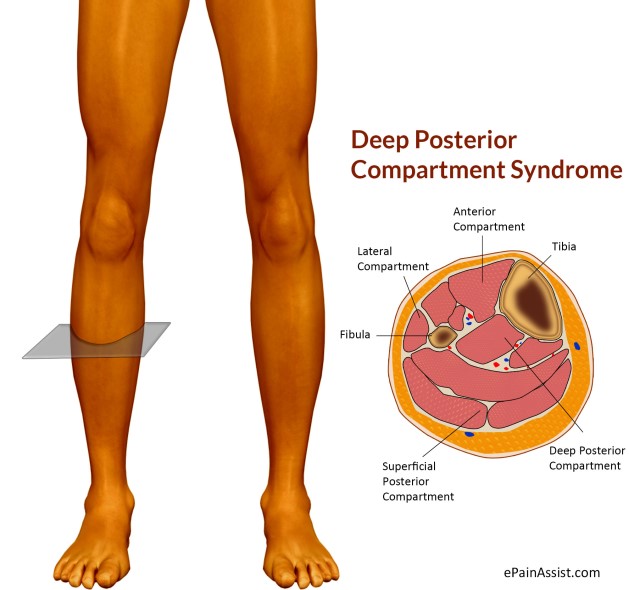
The tibialis posterior tendon becomes fibrotic through a process of repeated microtrauma. Some controversy remains about the underlying aetiology of this tendinosis.
A weak blood supply to the tendon has been identified as it courses behind the medial malleolus.
Mechanical factors must be at play that predispose the tendon to progressive fibrosis.
A growing body of research proposes that abnormal forces arise from even mild flat footedness, resulting in lifelong greater mechanical demands on the tibialis posterior than in a “normal” foot.
Another possible mechanical aetiology is overpull of the opposing peroneus brevis muscle. Rarely, rupture of the tibialis posterior tendon has also been associated with a traumatic event such as ankle fracture, ankle sprain, or a direct blow to the tendon.
It is important to point out that, although the tibialis posterior tendon may rupture, this is not necessary for tibialis posterior dysfunction to develop.
Classification
Johnson and Strom’s classification describes the progression of tibialis posterior dysfunction, and also serves as a guide to management.
Stage I dysfunction: the tendon is still intact and to some degree functioning, but it is inflamed.
Stage II dysfunction: the tendon has become dysfunctional and the foot has developed acquired flatfoot, but the deformity is passively correctable.
Stage III dysfunction: the foot deformity has become fixed, and degenerative changes are seen in the subtalar joint.
Stage IV dysfunction: occurs when degenerative changes are also present in the ankle joint.
Someone with a normal foot can perform a single heel rise eight to 10 times, but by stage II patients are unable (or barely able) to perform a single unsupported heel rise.
Even if the patient is supported to facilitate the attempted heel rise, the heel will not invert as it normally does (fig 3)
In stages III and IV, in addition to the findings in stage II, the flatfoot deformity has become fixed.
This is examined by grasping the heel and attempting to correct the valgus of the hindfoot
How to Examine for Tibialis Posterior Dysfunction

1. Both of patient’s legs visible from knee down
2. Observe heel alignment with patient standing with feet shoulder width apart, feet parallel. (Heel becomes valgus, arch collapses, and forefoot abducts in cases of tibialis posterior dysfunction)
3. Inspect for swelling behind medial malleolus
4. Ask patient to stand on tiptoes. Normally the heel should angle inwards. A patient with tibialis posterior dysfunction will have great difficulty standing on tiptoes, and the heel will not bend inward.
5. Ask the patient to perform 10 unsupported heel rises on each leg. A patient with tibialis posterior dysfunction will not be able to do this
6. Palpate along the tibialis posterior tendon for tenderness
7. Test tibialis posterior tendon for power. Ask the patient to bring foot into an inverted and plantar flexed position from an everted and dorsiflexed position against your resistance
8. Examine for hindfoot movement.
In stages I and II, the foot is supple and the flatfoot deformity can be corrected by rotating the heel inwards (the arch of the foot will be reconstituted).
In stage III and IV subtalar arthritis is present, and movement of the subtalar joint will be lessened and painful.
Additionally, in stage IV, ankle arthritis has set in and the ankle becomes stiff and painful.



Treatment
Conservative treatment is indicated for nearly all patients initially before surgical management is considered.
Compliance can be a problem, especially in stages I and II.
It helps to emphasise to the patients that tibialis posterior dysfunction is a progressive and chronic condition and that several fittings and a trial of several different orthoses or treatments are often needed before a tolerable treatment is found.
Stages I and II: the flexible foot Any acute inflammation surrounding the sheath of the tibialis posterior tendon should be dealt with before the chronic aspect of the condition is treated.
A period of four to eight weeks of immobilisation in a plaster cast below the knee or a removable boot (such as those made by Aircast) may be required to control accompanying inflammation.
In conjunction, RICE (rest, ice, compression, and elevation) and anti-inflammatories can be used, but steroid injection is contraindicated.

Footwear has an important role, and patients should be encouraged to wear supportive lace-up shoes, or even lace-up boots, which accommodate orthoses.
Stage I patients can try a laced canvas ankle brace before moving to a casted orthosis.
The various casted, semirigid orthoses support the medial longitudinal arch of the foot and either hold the heel in a neutral alignment (stage I) or correct the outward bent heel to a neutral alignment (stage II).
This approach is meant to serve several functions: to alleviate stress on the tibialis posterior; to make gait more efficient by holding the hindfoot fixed; and thirdly, to prevent progression of deformity.
Devices available to do this are the orthosis of the University of California Biomechanics Laboratory, an ankle foot orthosis, or a removable boot.
When this approach has been used, two thirds of patients have good to excellent results.
Stage III and IV: the rigid flatfoot overall, inflammation tends to be a less common feature of presentation with the rigid acquired flatfoot.
Treatment revolves around accommodating the deformity (rather than attempting to correct it) with customised moulded rigid orthoses, used in conjunction with appropriate footwear (often custom made), as the foot deformity worsens.
MAKE AN APPOINTMENT TO SEE ONE OF OUR FRIENDLY PODIATRISTS TODAY!



0 Comments